I. Epidemic Alert: High-Mortality Pathogen Sounds the Alarm Again
Recently, the Nipah virus (NiV) outbreak has once again occurred in West Bengal, India. As a priority pathogen under close surveillance by the WHO, the Nipah virus has garnered significant attention from the global scientific community due to its high case-fatality rate of 40%-75%, its lethality causing encephalitis, and its ability to transmit across species.
With no specific treatment or vaccine currently available, precise early diagnosis and antibody level monitoring are the only defenses against the spread of the epidemic. Bio-Mapper offers ready-to-ship key raw materials for the Nipah virus —— G protein (recombinant glycoprotein) and NP protein (nucleocapsid protein) —— to aid in global epidemic prevention.
II. Pathogenesis: The Central Role of G and C Proteins
During the infection process of the Nipah virus, G protein (glycoprotein) and C protein (nucleocapsid protein) play decisive roles.
• G protein (Glycoprotein) —— the “key” to invasion:
• Function: The G protein is responsible for recognizing and binding to the host cell surface receptors —— Ephrin-B2/B3.
• Mechanism: Ephrin-B2 is widely distributed in endothelial cells, the lungs, and the central nervous system, which explains why the Nipah virus causes severe encephalitis and respiratory diseases.
• Research/brand point: The G protein is the main antigen that induces the production of neutralizing antibodies and is a key target for vaccine development and antibody screening.

source:network
• Nucleocapsid NP protein (C protein) —— the “shield” of immune evasion:
• Function: The Nipah virus uses its P gene to encode non-structural proteins (including C, V, and W proteins) that interfere with the host’s innate immune response.
• Mechanism: The nucleocapsid protein shuttles between the cell nucleus and cytoplasm, effectively inhibiting the signaling of type I interferon (IFN), allowing the virus to evade detection in the host’s body initially and replicate rapidly.
• Research/brand point: Studying the nucleocapsid protein is crucial for understanding viral virulence and screening antiviral small-molecule drugs.

sorce:network
III. In-Depth Popular Science: The Hidden Differences Between Nipah Virus and Its “Relatives”
To achieve precise detection, it is essential to clarify the similarities and differences between the Nipah virus and its close relatives.
1. Nipah (NiV) vs. Hendra (HeV): The Divergent “Sister Viruses”
Both belong to the Henipavirus genus, but they differ in transmission and pathogenicity:
• Intermediate hosts: Hendra is mainly transmitted to humans through horses; Nipah is primarily transmitted to humans through pigs or food contaminated by fruit bats (such as raw date palm sap).
• Human-to-human transmission: Nipah virus (especially the Bangladeshi strain) has a clear risk of human-to-human transmission, while Hendra virus rarely transmits between humans.
• Clinical manifestations: Hendra tends to cause extreme acute respiratory distress; although Nipah also attacks the lungs, its most characteristic feature is the outbreak of encephalitis, leading to rapid patient coma.
2. Nipah vs. Measles/Mumps: Why Is Nipah More Lethal?
Although they belong to the same Paramyxoviridae family, the lethality of the Nipah virus far exceeds that of the latter two:
• Receptor breadth: The receptor (SLAM) bound by the measles virus is limited to immune cells. In contrast, the Nipah virus binds to Ephrin-B2/B3 receptors, which are highly conserved and widely present in endothelial cells throughout the body and neurons. This means that Nipah can launch a “systemic vasculitis” and “whole-brain attack.”
• Pathogenesis: The Nipah virus has a very strong immune evasion mechanism, capable of blocking the alarm signals of human interferon (IFN). By the time the immune system “realizes” the threat, the virus has already penetrated the blood-brain barrier, causing irreversible neurological damage.
IV. Vaccine Dilemma: Why Is There No Approved Human Vaccine Yet?
Current situation: There is currently only a Hendra vaccine for horses globally, with no approved human Nipah vaccine. Its development faces four major “hardcore” challenges:
• Extremely high biosafety level: Research must be conducted in BSL-4 (the highest level) laboratories, which are extremely scarce worldwide, limiting the speed of development.
• Ethical dilemmas in clinical trials: Nipah virus outbreaks are unpredictable and sporadic, and the mortality rate is too high. Conducting “randomized controlled trials” during outbreaks faces significant ethical controversies and operational difficulties.
• DIVA strategy challenge: The ideal vaccine needs to be combined with differential diagnosis (DIVA) to distinguish between natural infections and vaccine recipients, which requires extremely high precision for the accompanying diagnostic antigens (G vs. NP).
• Insufficient market drive: The epidemic mainly occurs in low-income areas, and international pharmaceutical giants have limited willingness to invest in research and development.
Note: In the evaluation of vaccine development, the G protein is the only key indicator for measuring the titer of neutralizing antibodies.
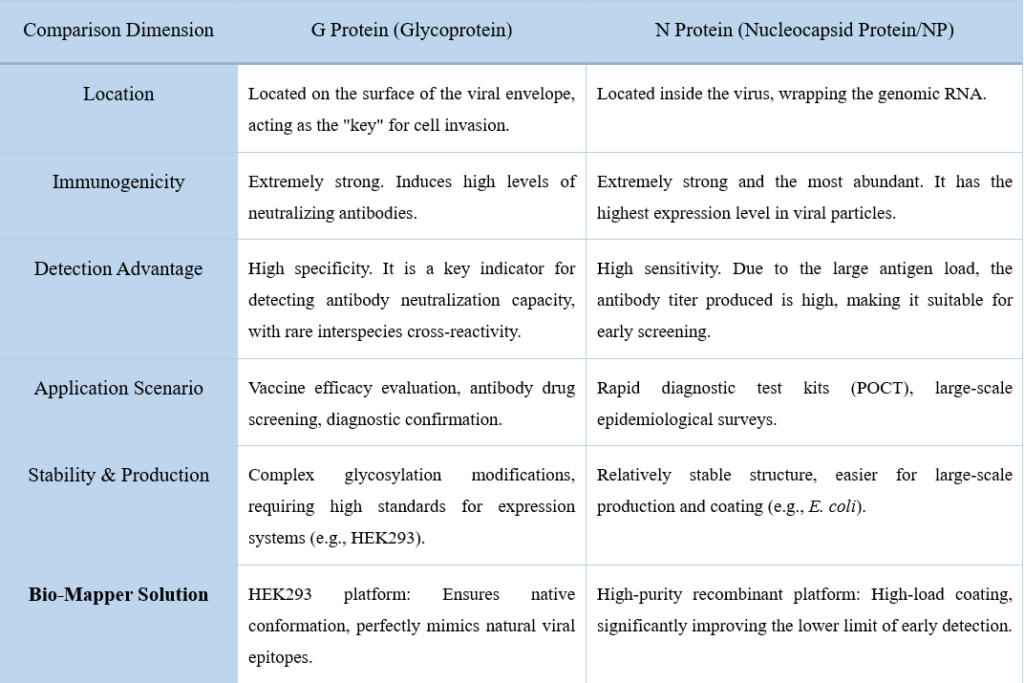
V. Diagnostic Strategy: The “Golden Combination” of G and NP Proteins
In the development of serological test kits, the choice of target antigens determines the sensitivity and specificity of the product. Here is a detailed comparison of the two core targets for Nipah virus:
Nipah Virus Diagnostic Target Comparison Table (G Protein vs. N Protein)
VI. Bio-Mapper : NiV Core Antigen Raw Material Solutions
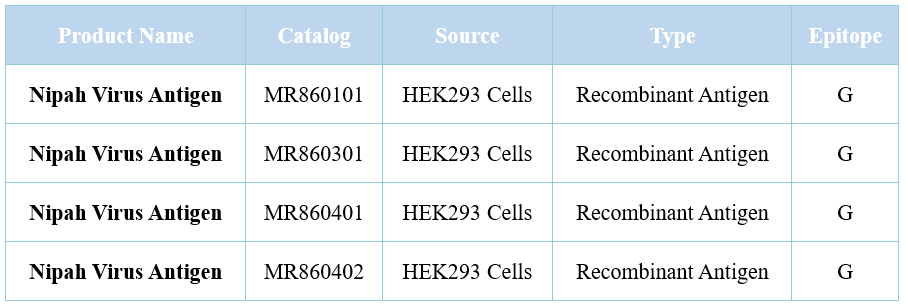
In response to the complex conformation of the Nipah virus, Bio-Mapper Bio ensures the natural glycosylation modification of the G protein through the HEK293 (mammalian cell) platform, providing you with superior raw material support:
1. Nipah Virus G Protein (for Specific Confirmation and Neutralization Assessment)
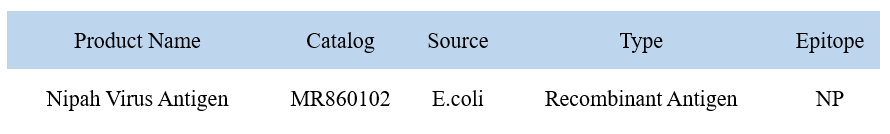
2. Nipah Virus NP Protein (Former C Protein, for Sensitive Screening)
VII. Prevention and Control Recommendations: What to Do When an Infected Person is Detected?
- Cut Off Transmission Routes: Avoid contact with fruit bats and refrain from consuming untreated raw date palm sap.
- Strict Isolation: Given that the Nipah virus can be transmitted between humans, suspected cases must be immediately placed under the highest level of individual isolation, and medical staff should wear level-three protective gear.
- Precision Monitoring: Collect serum or cerebrospinal fluid and use test kits developed with high-purity antigens from Bio-Mapper for early screening (NP) and confirmation (G).
Conclusion: Faced with the deadly Nipah virus, precise antigen raw materials are the cornerstone of scientific research and diagnosis. Bio-Mapper is committed to providing core weapons with stable performance to help combat global high-mortality infectious diseases.
For inquiries about technical details or to request samples, please contact your regional sales manager or leave a message in the backend!